What the heck is sciatica?
We hear, my sciatica is acting up all the time! But what the heck is sciatica anyways?!
As a chiropractor, there is not a day that goes by that I don’t hear the term “sciatica”! However, I hate the term! Why? Well, because its kind of a garbage term, that can mean so many things to so many different people. It’s really a symptom more than a true condition or diagnosis. Same as low back pain, low back pain is a symptom it’s not a diagnosis. Saying you have low back pain tells us nothing about WHY you have low back pain! Low back pain could be due to facet arthrosis, degenerative disc disease, a disc hernation etc., etc.
Sciatica, just means pain along the sciatic nerve, the largest nerve in our body that runs along the back of our thigh. Why many people have low back pain with sciatica, it does not mean low back pain. This is where people often misuse the term, and is reason #1 I hate the term. Sciatica, again just means pain along the sciatic nerve. The pain usually starts in the gluteal region better known as our butt. The pain sometimes will just stay in this area, but usually will travel down the back of our thigh, sometimes even crossing the knee.
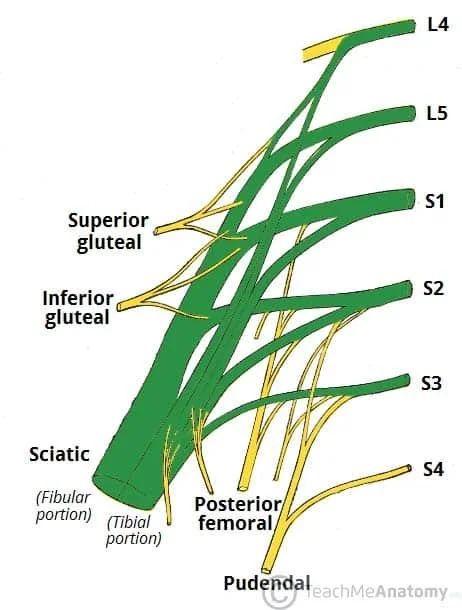
The sciatic nerve, is actually formed by SEVERAL spinal nerves in our lower back and can really be thought of as almost a continuation of the spinal cord. The sciatic nerve is actually formed by the lumbar nerves L4 and L5 and the sacral nerves S1-S3, meaning its actually made up of 5 spinal nerves! An issue at anyone of these levels therefore, could cause “sciatica”. This is reason #2 I hate the term! It describes a symptom, but tells us NOTHING about the CAUSE!
It would be like taking your car to the mechanic because it won’t start, and asking the mechanic what’s wrong? Only for them to tell you, your car won’t start! We already know the car won’t start, but the question is WHY? There are several reasons for why a car wont start, bad battery, out of gas, bad starter etc. That’s why “sciatica” is more of a symptom and less of a diagnosis, it doesn’t tell us the cause.
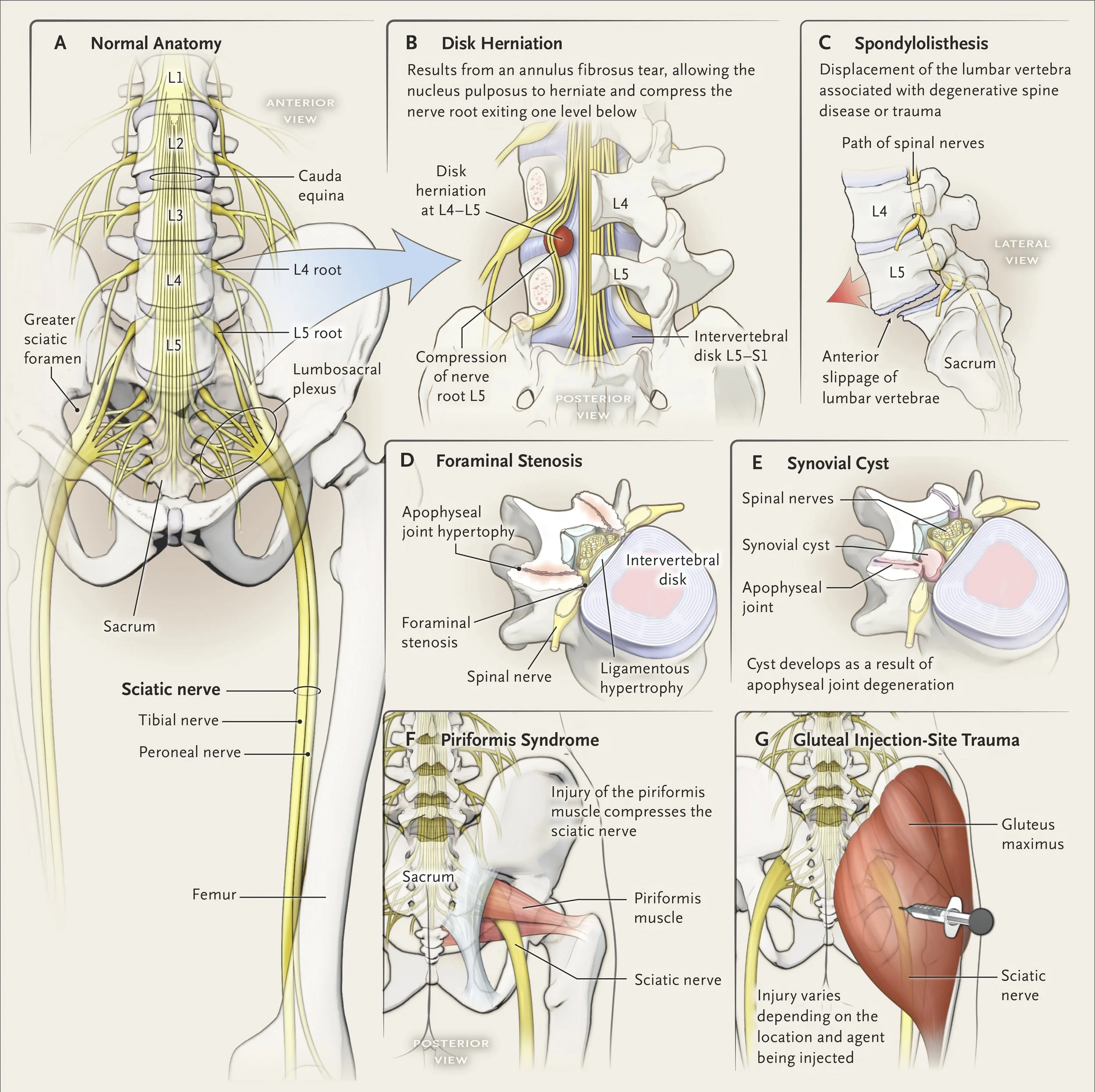
So what causes sciatica? Well, there can be multiple causes of sciatica… sometimes more than one is going on in a person at the same time. Overall, the leading cause of sciatica is a herniated disc. This accounts for an estimated 85% of all cases. A herniated disc is when disc material either the nucleus pulposus (jelly filling) or the annulus fibrosus (donut crust) extends beyond the normal shape of the disc and compresses one of the several nerve roots mentioned above.
In patients over 60, the number one cause of “sciatica”, is lumbar spinal stenosis, or narrowing of the spinal canal. This is because as we age, we are more likely to have osteoarthritis or wear and tear arthritis. This results in facet joint arthritis, ligamentum flavum hypertrophy, and spondylolisthesis(slipped vertebrae). These more degenerative changes that happen slowly overtime also lead to compression of one or more of the nerve roots which gives rise to the sciatic nerve.
Another, well-known cause of sciatica is what we call piriformis syndrome. The piriformis is a muscle located within our gluteal or butt region. It attaches from the outside of hip to the sacrum. The sciatic nerve either bases directly underneath this muscle or directly through this muscle. Therefore, when this muscle is tight, it can cause sciatica.
The following picture provides a great overview of normal anatomy involving the sciatic nerve, as well as a visual representation of the well-known causes of sciatica:
So you may be asking yourself, how do I or my doctor for that matter diagnose the CAUSE of MY SCIATICA? The majority of most if not all clinical diagnosis comes from a detailed patient history. Up to 90-95% of a diagnosis can come from the history alone. Understanding the onset, mechanism of injury, quality of pain, pattern of radiating pain, provocative factors and alleviating factors all help lead to a diagnosis of the root cause of the sciatica. The physical exam then either confirms or refutes the proposed diagnosis gathered from the initial patient history.
Imaging is NOT routinely indicated initially! Generally, spinal imaging in someone with radiating pain (sciatica) is reserved for those with symptoms that persists beyond 4-6 weeks, following a trial of conservative care such as chiropractic care, PT, acupuncture, etc.
The American College of Physicians (ACP) recommends nonpharmacologic treatment as first-line conservative management for acute or subacute sciatica. These recommendations include heat, massage, acupuncture or spinal manipulation! If medication is desired NSAIDs or muscle relaxants are generally recommended, while opioids such as hydrocodone or oxycodone are NOT recommended.
The ACP also recommends directional preference exercises (stretching in the direction that centralizes or abolishes pain) should be initiated alongside progressive aerobic exercise and management of kinesiophobia. In the subacute stage (6-12 weeks), neurodynamic mobilization and strength training should be added to the exercise regimen.
For chronic sciatica (>12 weeks), treatment should shift toward functional restoration combining spinal manipulative therapy with specific exercise and function-specific physical training.
Dr. Mike at Cole Spine and Performance, is well positioned to diagnose the root cause of your sciatica, and is well positioned to provide care that follows the above clinical practice guidelines. So if you suffer from sciatica consider scheduling appoint for further evaluation and treatment!
Here are some great exercises mentioned above in the guideline recommendations which may help relieve your sciatica:
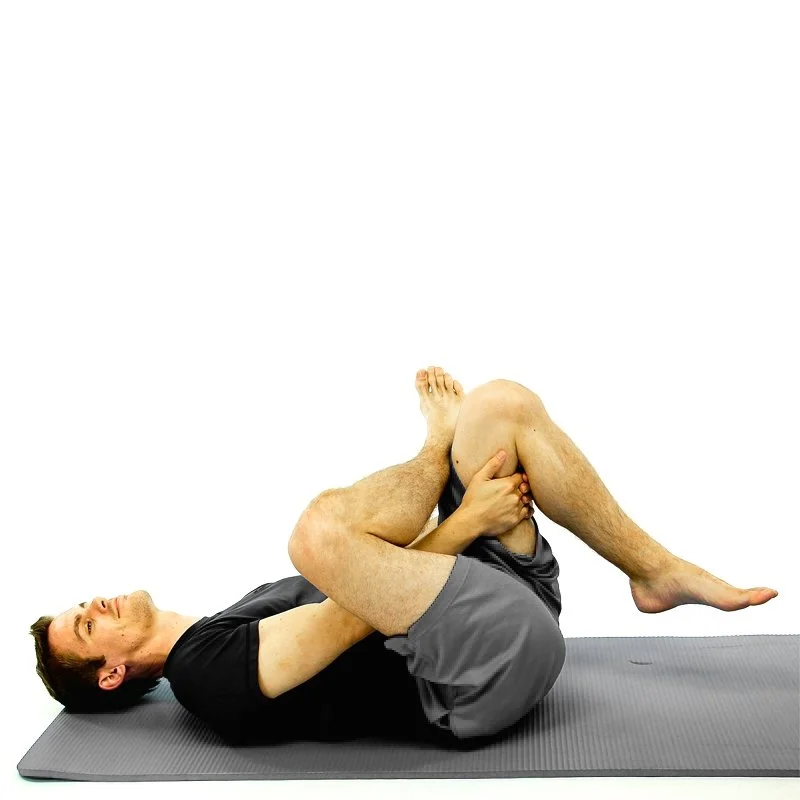
The above stretches are great at reducing tightness of the piriformis muscle which is often involved in sciatica. Even when the primary cause of the “sciatica” may be a disc herniation pressing on one of the nerves that forms the sciatic nerve. That’s because, compression of the nerve close to the spine can lead to neural inflammation, leading the rest of the nerve more prone to irritation and compression, known as double crush syndrome.
Next we will show you how to mobilize the nerve, also known as nerve gliding or nerve flossing. While the exact mechanism of how it works is not fully understood, it’s believed that moving the nerve back and forth helps to free it from being “pinched” and also helps to decrease the neural inflammation or inflammation of the nerve. I have seen this be very effective in patients even with severe lumbar stenosis or severe lumbar hernations.
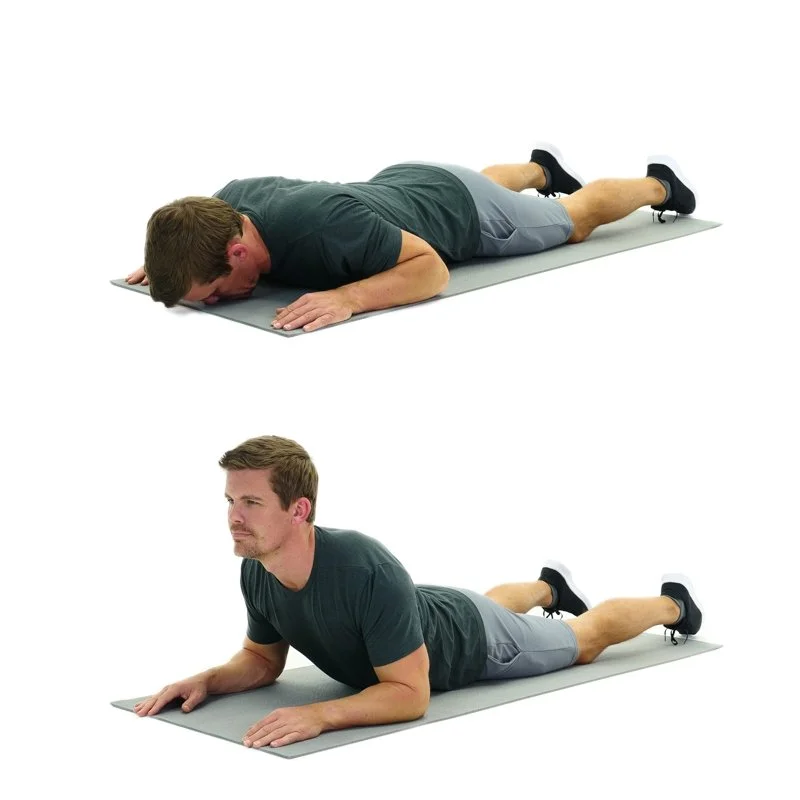
Lastly, we will discuss directional preference exercises also known as end-range loading or McKenzie Exercises, these terms are all relatively synonymous. It involves stretching in the direction that “centralizes” the pain. For most people, this is stretching into lumbar extension. That’s because a lot of us through out the day get forward slumped posture which increases pressure on the posterolateral disc, causing more irritation of the disc itself and or the nerve room. Stretching into extension, drives the pressure forward, alleviating the pressure on the disc, thus, resulting in decreased pain. You may experience a mild increase in low back pain, which is okay, as long as the pain becomes more centralized, meaning you start to experience less leg symptoms. While extension is most common, other planes of motion may also include stretching into flexion, or lateral flexion.
Still having issues?! Book an appointment for further evaluation and treatment!
Supine Piriformis Stretch: Lying on your back, cross the affected leg over in a figure-4 and pull the unaffected leg toward your chest (may use pillowcase or hand towel to help) Hold 20-30 seconds, repeat 2-3 reps 2-3x per day.
Resting Forearm Cobra: While laying on your stomach, come to rest on your elbows, causing your mid and low back to go into extension. Try and keep your bellybutton flat on the floor or table. Rest in this position for up to several minutes.
Seated Piriformis Stretch: Sitting upright cross the affected leg over in a figure-4 and gently press affected knee and flex at the hip inline with the bottom of the affected foot, hold 20-30 seconds, repeat 2-3 reps 2-3x per day.
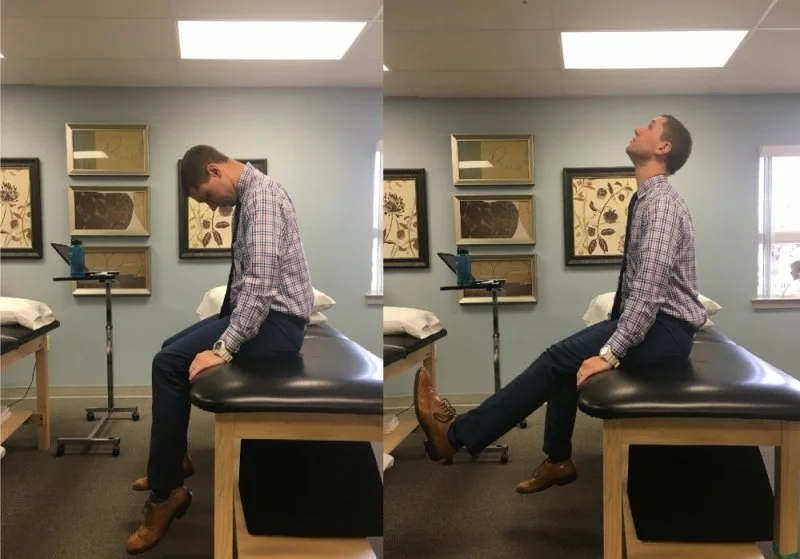
Seated Sciatic Nerve Flossing: Sitting upright look up while at the same time extend your knees and dorsiflex your ankle, pointing your toes toward your nose. Hold this for 5-seconds. After 5-seconds, look down while at the same time flexing your knee and plantar flexing your ankle or point your toes to the floor. Hold this for 5 seconds.
REPEAT 15 REPS 2-3X PER DAY!
Prone Press-Up: While laying on your stomach, extend your elbows similar to a push-up, but leave your bellybutton flat on the table or floor. Repeat 10-15 reps several times throughout the day or at onset of increased leg symptoms.
Seated cross-pull Piriformis Stretch: Sitting upright cross the affected leg over in a figure-4 and gently pull the affected knee to the opposite shoulder, hold 20-30 seconds, repeat 2-3 reps 2-3x per day.
Standing Lumbar Extension: While standing, place hands in small of back and extend back leaning into extension. Repeat 10-15 reps several times throughout the day or at the onset of increased leg symptoms.